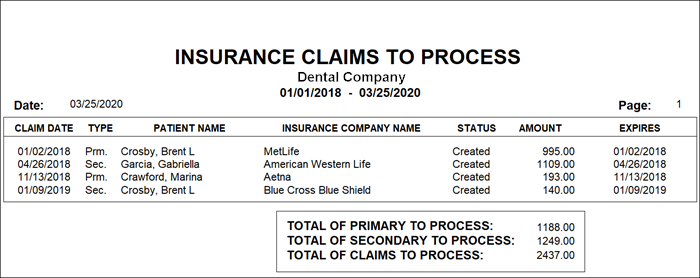
We all know that sometimes claims slip through the cracks and don’t get submitted, and running the Insurance Claims to Process report is the easiest way to catch them. This report will identify all insurance claims that have been created in the Accounts but not sent to the Batch Processor, or printed, or sent electronically through eClaims. (Note: the report will not show you claims that have been deleted.)
To find claims that haven’t been sent to insurance:
- Run the Insurance Claims to Process report. From Reports, click Account Reports > Insurance Claims to Process. Leave the patient, provider, and insurance carrier options set From <ALL> to <ALL> so that Easy Dental looks for all claims within the date range you specify. Click OK.
- Send claims as needed. Find the claims that need to be sent, go to that patient’s Account, and send the claims.
For more information, search for “Insurance Claims to Process” in Easy Dental Help.




